In this unprecedented time, the simple act of going to the doctor seems scary. We are all asking ourselves, is the risk of contracting Coronavirus (COVID-19) during a routine prenatal visit worth the benefit of the appointment? And if a pregnant patient happens to have COVID-19, could she infect other women, or the frail and vulnerable patients who are in the hospital or medical office building at the same time?
Almost all prenatal care is about prevention or diagnosis. It’s almost never about treatment. We measure weight and blood pressure to make sure mom isn’t developing a hypertensive disorder. We measure the belly or use ultrasound to make sure the fetus is developing normally. We send laboratory tests to rule-out other conditions. We almost never provide medication that can’t be dispensed from the local CVS.
In these times, we are rethinking routine prenatal care for low-risk women. Home monitoring of weight and blood pressure combined with ‘check-ins,’ by telephone could replace many routine prenatal visits. Liberal use of kick-counting and technology-based remote clinical supervision could insure that mom and her fetus remain healthy, while protecting her from preventable infection.
In a survey of 2,200 women conducted March 25-27, fewer than 25 percent of prenatal care visits were being modified; this number should probably be 50 percent.
Of course patients with hypertension or diabetes, those at risk for fetal loss, and women who have other high-risk conditions will need to be seen in person on a routine basis (although maybe not as frequently as they are being seen now).
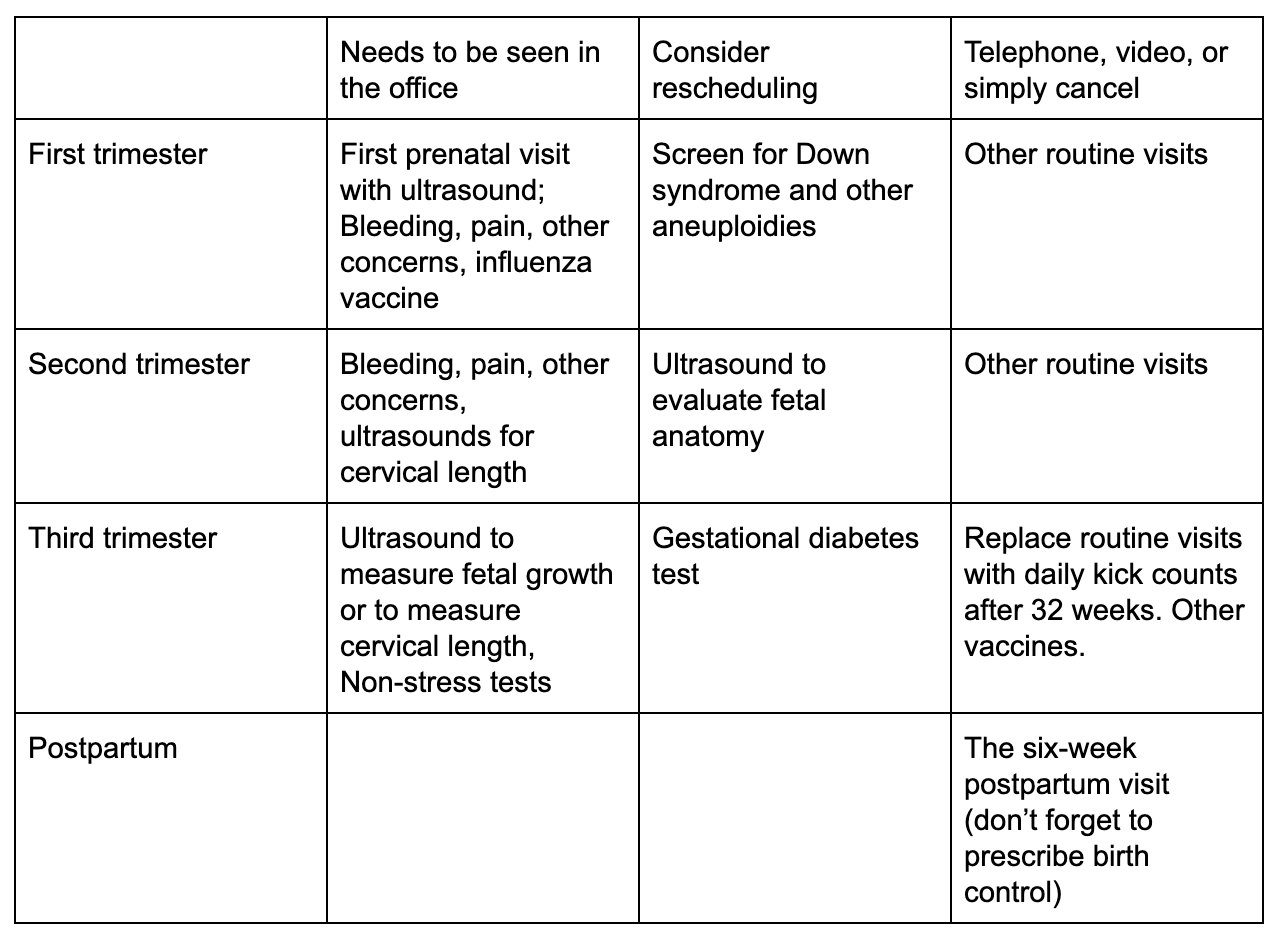
Here’s one approach to rethinking prenatal care in the era of a community contagion (for low-risk patients only):
This approach isn’t for high-risk patients, and it would certainly feel strange for women and their healthcare providers. Providers are concerned about technology - how to visit patients online and how to document those visits - as well as payment coverage for nontraditional visits. However, telehealth services are well-established, and most OBGYNs and midwives have colleagues who can help them get up to speed quickly.
To my obstetric colleagues:
Consider which visits can go online or be handled by phone, and schedule them that way.
Can some visits be safely cancelled? Do it!
Encourage your patients to purchase (or better yet, order online) scales and home blood-pressure cuffs
Help your staff to create a home-prenatal care guide from your office that includes instructions on kick counting (or use Ovia’s kick-counter here), and COVID-19 symptoms.
To our pregnant patients:
Use the chart above to ask your healthcare provider if you can schedule your (appropriate) prenatal visit by phone or online
Check-in by phone before going to any in-office or hospital visits
Consider ordering the tools you will need to be your own prenatal care advocate at home, beginning with a scale and blood pressure cuff.
Some prenatal visits for some patients are critical to the health of both mom and baby, and hospitals are doing a valiant job assuring that they can take place safely. Our job now is best align safe prenatal care with COVID-19 prevention practices.